Navigating healthcare can be complex, especially for seniors. A common concern is whether Medicare covers medical transportation services. The good news is that Medicare does provide coverage for certain types of transportation, particularly in emergent situations or when medically necessary.
Understanding how these transportation services work is vital for your healthcare planning. You’ll find that coverage can vary significantly based on your specific Medicare plan. This is where The Modern Medicare Agency can assist you. Our licensed agents are available for one-on-one consultations, helping you identify Medicare packages that suit your needs without extra fees.
Knowing your options for medical transportation can enhance your access to necessary healthcare. With our expertise, you can be confident in finding the best solutions tailored to your unique situation.
Medicare Coverage for Medical Transportation Services
Navigating the intricacies of Medicare coverage for medical transportation can be challenging. Understanding what qualifies for coverage, the eligibility requirements, and the differences between emergency and non-emergency services can help you make informed decisions about your healthcare.
What Qualifies as Medical Transportation
Medical transportation under Medicare typically includes services essential for reaching medical appointments. This primarily involves emergency transportation, such as ambulance services, covered under Medicare Part B.
Non-emergency transportation may also qualify if it is medically necessary, such as for individuals needing regular treatments like dialysis. Original Medicare does not usually cover transportation for convenience, like trips to the gym or social gatherings.
Eligibility Criteria for Medicare Transportation Coverage
Eligibility for medical transportation services generally requires that transportation must be medically necessary. This means a healthcare provider must validate that providing transportation is essential for receiving medical care.
Medicare Part B covers ground ambulance services in emergencies. For non-emergency situations, your Medicare Advantage plan may offer additional options, but coverage details can vary widely.
To qualify, you need to be a Medicare beneficiary, and specific documentation from your healthcare provider may be required.
Differences Between Emergency and Non-Emergency Transportation
Emergency transportation is covered under Medicare when it’s necessary to get you to a hospital or skilled nursing facility. This coverage ensures quick response and transport in life-threatening situations.
Non-emergency transportation requires a higher level of documentation to validate the medical necessity. This can include rides to scheduled medical appointments or treatment sessions. Keep in mind that not all Medicare plans provide the same benefits for non-emergency transport, so checking with your plan is crucial.
For seniors navigating their Medicare options, The Modern Medicare Agency offers personalized assistance. Our licensed agents are available for one-on-one consultations to help you find the Medicare plan that best fits your needs without any unexpected fees.
Emergency Ambulance Transportation Under Medicare
Medicare provides specific coverage for emergency ambulance transportation, ensuring that beneficiaries receive critical medical services when needed. This section outlines the coverage details for ground and air ambulance services, as well as any limitations imposed on these emergency transportation options.
Ground Ambulance Services
Medicare Part B covers ground ambulance services for emergency situations. You qualify for coverage when the ambulance is necessary to transport you to a hospital, critical access hospital, or skilled nursing facility. This occurs when other forms of transportation might endanger your health.
Costs are structured with a coinsurance of 20% after you meet the annual deductible, which is $257 in 2025. It’s crucial to choose a Medicare-approved ambulance service. Confirming this can help minimize out-of-pocket costs.
Air Ambulance Coverage
Air ambulance services are covered only under specific conditions. Medicare may approve coverage if you need urgent medical treatment and ground transportation would take too long or jeopardize your health. This includes transport via helicopters or airplanes to the nearest appropriate medical facility.
Like ground services, beneficiaries are responsible for 20% of the Medicare-approved amount after the deductible. It’s essential to verify that the air ambulance service is a participating provider to avoid unexpected costs.
Limits on Emergency Transportation
There are limitations on what Medicare covers regarding emergency ambulance services. For example, transportation to a facility for non-emergency reasons, such as routine check-ups, is typically not covered. Additionally, coverage only applies to medically necessary instances.
Medicare does not cover expenses when you choose a non-emergency ambulance for convenience. Understanding the specific criteria and ensuring your emergency transportation needs align with Medicare coverage will help you avoid out-of-pocket expenditures.
For tailored Medicare guidance, consider choosing The Modern Medicare Agency. Our licensed agents work with you one-on-one to find the right Medicare packages without hidden costs, ensuring you receive the support you need.
Non-Emergency Ambulance and Medical Transportation
Understanding the specifics of non-emergency ambulance and medical transportation services is essential for managing your healthcare needs under Medicare. These services can provide critical assistance for scheduled medical appointments when more conventional transportation may not be suitable.
Medically Necessary Non-Emergency Ambulance Transport
Medicare Part B covers non-emergency ambulance services when they are deemed medically necessary. This means that the transportation must be required to obtain medically necessary care, and using other forms of transport could jeopardize your health.
Examples of situations where this applies include needing treatment for chronic pain or undergoing scheduled procedures. Ensure that all trips are documented and that the necessity of ambulance transport is clear.
Requirements for Doctor’s Orders and Prior Authorization
For non-emergency ambulance transportation to be covered, a doctor’s order is usually required. This order should specify the medical need for transport and detail the patient’s health condition.
In some cases, prior authorization is needed. This means you’ll need to obtain approval from Medicare before the service is provided. You can receive an Advance Beneficiary Notice (ABN) if there is uncertainty about coverage. An ABN helps you understand your financial responsibility if services aren’t covered.
Coverage for End-Stage Renal Disease and Dialysis Trips
Beneficiaries with End-Stage Renal Disease (ESRD) have additional coverage options. Medicare typically covers medically necessary transportation for dialysis treatments. This includes both emergency and non-emergency transport, ensuring that you can attend your sessions reliably.
To facilitate this, you may use non-emergency ambulance services when required, provided that they meet Medicare’s conditions for medical necessity. Understanding the coverage for your unique situation is vital, and expert guidance can be invaluable.
At The Modern Medicare Agency, our licensed agents offer personalized support. They will help you navigate Medicare packages that meet your healthcare needs, ensuring that you receive the right coverage without unexpected fees.
Medicare Advantage and Supplemental Transportation Benefits
Medicare Advantage plans, also known as Medicare Part C, often provide enhanced transportation benefits that are not available through Original Medicare. Understanding what these plans cover regarding transportation can help you make informed decisions about your healthcare needs.
What Medicare Advantage Plans May Offer
Many Medicare Advantage plans include transportation services as part of their benefits. These services can cover rides to medical appointments, therapy sessions, and sometimes even fitness centers.
Some plans may utilize rideshare services like Lyft or Uber for non-emergency transportation. This modern approach adds flexibility and convenience for enrollees, especially for those with mobility challenges. It’s essential to review your specific plan details, as coverage can vary considerably from one provider to another.
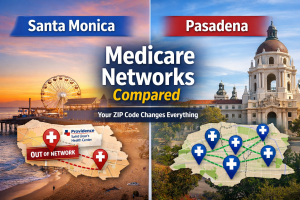
Comparing Medicare Advantage and Original Medicare Coverage
Original Medicare primarily covers emergency ambulance transportation. This means you might not have funds available for non-emergency transport, which is where Medicare Advantage shines.
With Medicare Advantage, you can access a broader range of transportation options, including scheduled trips to doctors and specialists. Many plans provide a defined number of rides per year, often at little or no cost to you. This benefit can alleviate the stress of arranging transport and ensure you receive necessary medical care.
Role of Medigap in Covering Transportation Costs
Medigap plans, also known as Medicare Supplement plans, can complement Original Medicare. However, they do not typically cover the additional transportation benefits available through Medicare Advantage plans.
If you have a Medigap policy, it will help with some out-of-pocket costs related to Medicare services but won’t address non-emergency transportation. If you rely heavily on transportation for your medical needs, evaluating a Medicare Advantage plan may be more beneficial.
Choosing the right plan can be complicated. At The Modern Medicare Agency, our licensed agents provide personalized assistance to help you find the right Medicare package that meets your needs without extra costs.
Costs, Limitations, and Accessing Medicare Transportation Services
Understanding the costs and limitations related to Medicare transportation services is crucial for ensuring you receive necessary medical care. This includes being aware of your financial responsibilities and knowing how to access these services properly.
Part B Deductible and Coinsurance Responsibilities
When using Medicare for medical transportation, you must consider the Part B deductible and coinsurance. For 2025, the Part B deductible is typically around $226 annually. Once this is met, Medicare generally covers 80% of the approved amount for ambulance services. You are responsible for the remaining 20%, which is known as coinsurance.
If your transportation for medical services does not meet Medicare’s strict criteria, you could face additional costs. Understanding these financial obligations helps you plan for unexpected expenses. Contacting The Modern Medicare Agency can help clarify these costs and assist you in comparing plans that suit your needs without any hidden fees.
Medicare-Approved Amount and Additional Expenses
Medicare only covers ambulance services when they are medically necessary. This means that if you require a ride to your appointment, you must demonstrate that other transport options could pose a risk to your health. The Medicare-approved amount for ambulance services can vary by location and provider, depending on agreements with ambulance companies.
If an emergency service requires prior authorization, be prepared for delays if you don’t submit documentation promptly. Additionally, you might receive an Advance Beneficiary Notice (ABN) if a service isn’t likely to be covered, alerting you to potential out-of-pocket costs. Always check in with your provider to ensure you understand your responsibilities.
How to Arrange Covered Medical Transportation
Arranging medical transportation through Medicare can be straightforward. Start by confirming with your healthcare provider that the service will be covered and meets Medicare’s criteria. If you require an ambulance, ensure it is a provider that accepts Medicare.
In many cases, you’ll need to provide medical documentation that justifies the need for ambulance services. If you are not eligible for ambulance transport, consider contacting local area agencies on aging for alternative options. They may offer free or low-cost services tailored to seniors. For the best advice on navigating these arrangements, reach out to The Modern Medicare Agency, where licensed agents will guide you through the process efficiently.
Alternative and Community-Based Transportation Resources
When Medicare does not provide adequate transportation coverage, you may access alternative solutions. Various state Medicaid programs and local initiatives can bridge the gap for those in need of medical transportation. Community organizations and ride-sharing partnerships also offer viable options for getting to appointments and healthcare services.
State Medicaid and Local Transportation Programs
State Medicaid programs often include Non-Emergency Medical Transportation (NEMT) services. These programs help eligible individuals reach medical appointments, particularly for those facing financial hardships.
To utilize these services, contact your local Medicaid office or area agency on aging to understand your eligibility. Often, these programs will cover:
- Private car services
- Ambulance transport in specific cases
- Public transportation vouchers
Local agencies may also have additional resources or partner with transportation providers to ensure service availability. For instance, some regions have designated taxi services or shuttles for medical appointments, making access easier for seniors and those with disabilities.
Community Organizations and Ride-Sharing Partnerships
Various community organizations offer transportation support tailored to their local populations. Many of these groups work with ride-sharing services to create affordable options for patients needing rides to healthcare facilities.
For example, you might find:
- Volunteer drivers from local non-profits willing to assist individuals with rides.
- Partnerships with ride-sharing platforms providing discounts or special services for medical appointments.
Programs may vary, so check with your local agencies for options. These community resources often prioritize low-cost solutions, ensuring you can attend essential healthcare appointments without significant financial strain.
If you’re navigating these options, consider The Modern Medicare Agency. Our licensed agents provide personalized assistance to identify Medicare packages that best suit your transportation needs without hidden fees.
Frequently Asked Questions
Understanding Medicare’s coverage for medical transportation services involves various aspects, including specific types of transport, conditions for coverage, and reimbursement details. Here are some key points regarding Medicare’s transportation benefits.
What types of transportation services are covered under Medicare?
Medicare covers emergency ambulance services when medically necessary. This can include transport to hospitals, critical access hospitals, or skilled nursing facilities when other transportation could endanger your health. Non-emergency transportation is not typically covered under Original Medicare.
Can Medicare beneficiaries receive coverage for non-emergency medical transportation?
Medicare does not usually cover non-emergency medical transportation under Original Medicare. However, some Medicare Advantage plans may offer benefits for transportation to non-emergency medical appointments. You should check the specific coverage details of your plan for more information.
Are there any conditions that must be met for Medicare to cover ambulance services?
Yes, Medicare requires specific conditions to be met for ambulance services coverage. You must have a medical necessity for the service, meaning that any other form of transport could jeopardize your health. Additionally, Medicare will cover only ground ambulance services, typically when a doctor prescribes it.
How does Medicare coverage vary for transportation to routine medical appointments?
Original Medicare does not cover routine transportation to medical appointments. If you have a Medicare Advantage plan, some plans may provide transportation benefits for scheduled visits, but this varies by provider. Always review your plan details to understand available benefits.
Will Medicare Part B reimburse the costs of transportation for medical purposes?
Medicare Part B covers emergency ambulance transportation when it is medically necessary. However, reimbursement is conditioned upon strict criteria. If other means of transportation endanger your health, Medicare may reimburse the costs associated with the ambulance services.
Does Medicare offer any coverage for transportation assistance for disabled individuals?
Medicare does not specifically provide coverage for transportation assistance for disabled individuals. Coverage is mainly for emergency medical transportation. However, individuals may explore Medicare Advantage plans, which sometimes include additional transportation benefits, depending on policy specifics.
At The Modern Medicare Agency, you’re not just a number. Our licensed agents are real people who can help you navigate the complexities of Medicare. We work with you to identify plans that meet your needs without hidden fees. Let us guide you through your Medicare insurance journey.