You want to know the difference between Medigap and Medicare Part C so you can pick the right plan for your health and budget. Medigap supplements Original Medicare to help pay deductibles and coinsurance and lets you see any doctor who accepts Medicare, while Medicare Part C (Medicare Advantage) replaces Original Medicare with a bundled plan that often limits you to a network but can add extra benefits.
This piece will show how those trade-offs affect your care, costs, and flexibility. Deciding gets easier when you have clear guidance.
The Modern Medicare Agency helps you compare options with licensed agents you can talk to one-on-one. They help find plans that match your needs and avoid extra fees.
Understanding Medigap
Medigap helps pay gaps in Original Medicare costs like deductibles, copays, and coinsurance. It lets you see any doctor who accepts Medicare and works alongside Part A and Part B to reduce your out‑of‑pocket spending.
What Medigap Covers
Medigap policies fill specific cost gaps left by Original Medicare. Common benefits include paying all or part of:
- Part A hospital coinsurance and hospital costs after Medicare benefits end
- Part B coinsurance or copayments
Other covered costs can include the Part A deductible and skilled nursing facility coinsurance (for some plans). Some plans also cover emergency care when you travel outside the U.S.
Medigap does not cover prescription drugs, so you’ll need a separate Part D plan if you want drug coverage. Benefits are standardized by plan letter in most states, so a Plan G from one insurer must match Plan G from another in what it pays.
Who Is Eligible for Medigap
You qualify for Medigap if you have Original Medicare (Part A and Part B). You cannot use Medigap with Medicare Advantage (Part C) at the same time.
You get the best enrollment rights during your Medigap Open Enrollment Period, which starts the month you turn 65 and have Part B. During this six‑month window, insurers must accept you regardless of health issues in most states.
If you enroll later, insurers can use medical underwriting and may charge higher premiums or deny coverage. You must buy your own Medigap policy; your spouse needs a separate policy.
Types of Medigap Plans
Medigap plans use letters (A, B, C, etc.) to show what they cover. Each lettered plan in the same state offers the same basic benefits no matter which insurance company sells it.
Common popular plans include:
- Plan G: covers most out‑of‑pocket costs except the Part B deductible.
- Plan N: lower premiums but requires small copays for some doctor and emergency visits.
Not all plans are available to new enrollees; for example, Plan F is closed to people who first became eligible after 2020. Premiums vary by insurer, age, and location even though benefits match by letter.
Understanding Medicare Part C
Medicare Part C bundles your Part A and Part B benefits through private insurers. It often adds benefits like prescription drugs, vision, or dental, and it uses networks and prior authorizations to manage care and costs.
What Medicare Part C Covers
Medicare Part C, also called Medicare Advantage, replaces Original Medicare (Parts A and B). It must cover everything Part A and Part B cover, such as hospital stays, doctor visits, and outpatient care.
Many plans add prescription drug coverage (Part D), routine vision, dental, hearing, and wellness programs. Costs vary by plan.
You typically still pay the Part B premium plus any Medicare Advantage plan premium. Plans set their own rules for copays, coinsurance, and deductibles.
Prior authorization may be required for some services. Part C plans often limit care to a network of doctors and hospitals, so check provider lists before you join.
Who Can Enroll in Medicare Part C
You can enroll in Medicare Part C if you have Medicare Part A and Part B and live in the plan’s service area. You cannot enroll in a Medicare Advantage plan if you only have Part A or Part B alone.
Some people with End-Stage Renal Disease (ESRD) may qualify for certain plans, but rules vary by year and plan. Enrollment windows matter.
You can join when you first become eligible for Medicare, during the Annual Enrollment Period (Oct 15–Dec 7), or in special election periods if you qualify. If you drop Part B, you usually cannot join Part C.
Types of Medicare Advantage Plans
Medicare Advantage plans come in several common types.
- HMOs (Health Maintenance Organizations): Require you to use in-network providers and get referrals for specialists.
- PPOs (Preferred Provider Organizations): Let you see out-of-network providers at a higher cost without referrals.
Other types include:
- PFFS (Private Fee-for-Service): Let the plan set payment rules; provider acceptance can vary.
- SNPs (Special Needs Plans): Serve people with specific health needs, like chronic conditions or institutional care.
Each type affects cost, flexibility, and provider choice. Compare network size, drug formularies, and prior authorization rules.
Key Differences Between Medigap and Part C
Medigap fills gaps in Original Medicare benefits, while Part C bundles Medicare benefits and often adds extras. Costs, provider access, and how you use care differ a lot between the two.
Coverage Differences
Medigap supplements Original Medicare (Part A and B). It pays out-of-pocket costs like deductibles, coinsurance, and some excess charges depending on the Medigap plan you choose.
You keep Original Medicare and can see any provider that accepts Medicare without needing referrals. Part C, or Medicare Advantage, replaces Original Medicare with a private plan.
It includes Part A and B benefits and often Part D drug coverage plus extras like dental or vision. These plans can limit coverage to in-network providers and may require prior authorization for some services.
Cost Structure Comparison
Medigap plans usually charge a monthly premium in addition to your Part B premium. You pay predictable costs because Medigap covers many out-of-pocket risks.
Some Medigap plans have higher monthly premiums but lower unexpected costs. Part C plans often have lower monthly premiums or even $0 premiums, but you may face copays, coinsurance, and an annual maximum out-of-pocket limit.
Your total yearly cost depends on how much care you use and whether you must stay in a network. Compare plan premiums, expected medical use, and out-of-pocket caps.
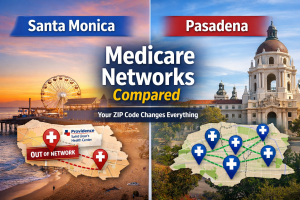
Provider Network Access
With Medigap, you can see any doctor or hospital that accepts Medicare anywhere in the U.S. That makes Medigap a strong choice if you travel or use multiple specialists.
Part C plans commonly use networks: HMOs, PPOs, or provider lists. Staying in-network usually costs less.
Going out-of-network can mean higher costs or no coverage for some services. Check each plan’s network rules before you enroll.
Enrollment and Eligibility Considerations
You need to know when you can join or change plans and what rules affect your choices. Timing, guaranteed issue rights, and prior coverage all matter for whether you qualify and how much you pay.
Open Enrollment Periods
Your initial Medigap Open Enrollment starts the month you turn 65 and have Part B, and it lasts six months. During this window, insurers must sell you any Medigap policy without charging more for preexisting conditions.
If you miss this period, companies can use medical underwriting and may deny coverage or charge higher rates. Medicare Advantage (Part C) has different windows.
You can join a Part C plan when you first enroll in Medicare or during the Annual Election Period (Oct 15–Dec 7). You also get a Medicare Advantage Open Enrollment (Jan 1–Mar 31) to switch or drop plans once each year.
Note that switching into a Medigap plan after you leave Part C can be tricky and may require underwriting.
Switching Between Plans
You cannot have Medigap and Medicare Advantage at the same time. If you leave a Part C plan and want Medigap, you might face a medical review unless you have a guaranteed issue right.
Common guaranteed issue situations include losing employer coverage or your Part C plan ending its contract with Medicare. When you move from Medigap to Part C, you generally keep your Medigap policy only if you cancel it first — which can leave gaps in coverage.
Speak with an agent before you switch to understand timing, possible coverage gaps, and costs.
Additional Benefits and Limitations
Medigap and Medicare Part C differ mainly in what they add to Original Medicare and what they leave out. One focuses on filling gaps in Original Medicare, while the other replaces it and often bundles extra services.
Prescription Drug Coverage Options
Medicare Part C (Medicare Advantage) often includes Part D prescription drug coverage as part of the plan. This means you can get medical and drug coverage in one plan.
Check each plan’s formulary, tiers, and copays because costs and covered drugs vary by insurer and plan network. Medigap plans do not include drug coverage.
If you choose Medigap, you must buy a separate Part D plan for prescriptions. Compare Part D lists and costs carefully to avoid gaps or high out-of-pocket drug costs.
If you need help comparing drug formularies or matching a Part D plan with a Medigap policy, The Modern Medicare Agency can help.
Extra Services and Perks
Medicare Advantage plans commonly offer extra services such as dental, vision, hearing, and fitness benefits. These extras can include routine cleanings, eyeglass allowances, hearing exams, and gym memberships.
Availability and limits vary by plan and region, so check exact benefit amounts and provider networks. Medigap focuses on covering out-of-pocket costs like deductibles and coinsurance.
It generally does not offer dental, vision, or hearing perks. You can buy stand-alone dental or vision plans if you want those services, but those add extra premiums.
Choosing the Right Plan for Your Needs
You need clear trade-offs: whether you want predictable costs and national doctor access, or lower premiums with network-based benefits and extra services. Think about your budget, doctors, prescription needs, and travel habits.
Factors to Consider
Look at these specific items when comparing Medigap and Part C (Medicare Advantage):
- Monthly cost vs. out-of-pocket risk
- Medigap: higher monthly premium, low or no cost sharing.
- Part C: lower premium often, but copays, coinsurance, and an annual max out-of-pocket can add up.
- Provider access
- Medigap: see any provider that accepts Medicare nationwide.
- Part C: often requires using a plan network or getting referrals for specialists.
- Prescription drug coverage
- Medigap: buy a separate Part D plan for drugs.
- Part C: many plans include Part D built in.
- Extra benefits
- Part C may include dental, vision, or hearing at no extra cost.
- Medigap generally does not include these extras.
- Travel and relocation
- If you travel or split time between states, Medigap keeps your provider options steady.
- Part C can limit coverage outside your plan area.
Making an Informed Decision
Gather concrete facts before you choose:
- Compare actual numbers: list premiums, deductibles, copays, and the plan’s annual out-of-pocket maximum.
- Check provider lists: confirm your primary doctors and preferred hospitals accept the plan or are in-network.
- Review drug coverage: match your current prescriptions to the plan’s drug formulary and costs.
Use these practical steps:
- Create a one-page comparison showing expected yearly cost for each option.
- Call The Modern Medicare Agency to speak with a licensed agent 1-on-1.
Our agents run side-by-side cost and provider checks based on your zip code and prescriptions.\ 3. Ask about enrollment rules, trial periods, and how to switch plans if your needs change.
Our agents identify plans that match your needs without adding hidden fees.\ You get clear numbers and a real person to answer follow-up questions.
Conclusion
You now know Medigap fills gaps in Original Medicare.
Part C (Medicare Advantage) replaces Original Medicare with a bundled private plan.
Each path affects costs, networks, and flexibility in different ways.
Choose Medigap if you want predictable out-of-pocket costs and wider provider choice with Original Medicare.
Choose Part C if you prefer one plan that may include extra benefits and lower premiums but may limit which doctors you can see.
Our licensed agents are real people you can speak with one-on-one.
They listen to your needs and find Medicare packages that match your budget and care preferences.
You don’t pay extra fees for help.
You get clear comparisons and plain answers so you can decide with confidence.