The buzz is real. GLP-1 medications like Wegovy, Ozempic, Zepbound, Mounjaro are everywhere. Between social media, headlines, and friends talking, many are asking: Will Medicare cover these weight-loss drugs? And should I use them?
Here’s the honest truth—what is covered now, potential changes, what GLP-1s do, the pros & cons, and why for many, diet + exercise are still powerful, safer tools.
What Medicare Currently Covers
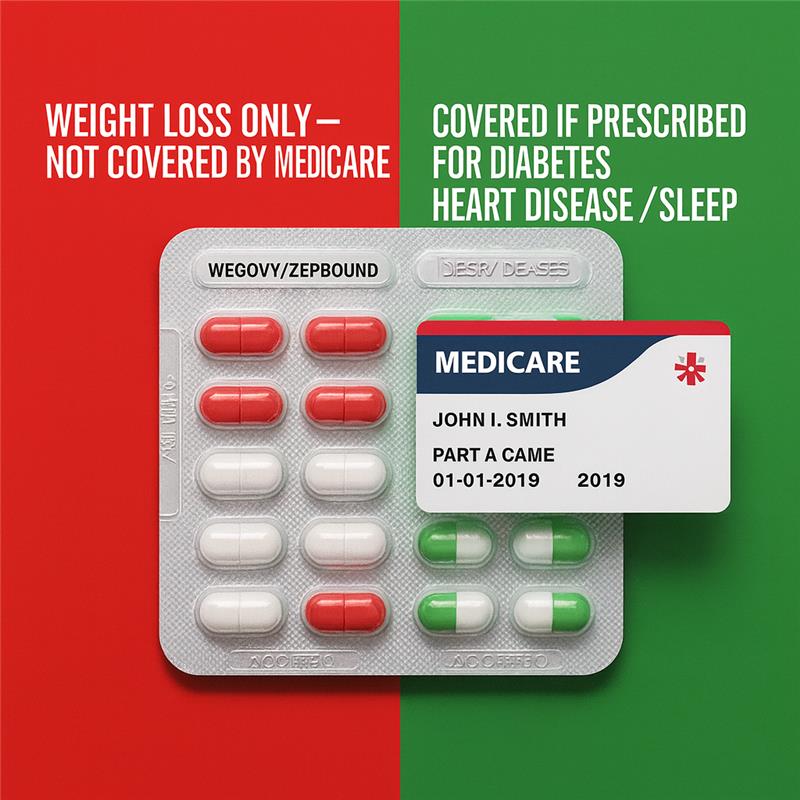
Legal & policy barriers still prevent Medicare from broadly covering GLP-1 drugs solely for weight loss. Here’s what is true for 2025-2026:
Medicare Part D plans are only allowed to cover GLP-1 drugs if they are prescribed for an FDA-approved indication other than just “weight loss.” For example:
-
Treating type 2 diabetes. (ASPE)
-
Reducing risk of major adverse cardiovascular events (MACE) in adults with obesity or overweight and established cardiovascular disease—when the drug has that indication (e.g. Wegovy got that approval in 2024). (U.S. Food and Drug Administration)
-
Potentially treating obstructive sleep apnea (OSA) if approved and prescribed accordingly. Some GLP-1s (e.g., Zepbound) are being studied or already approved for non-weight-loss uses like this. (KFF)
What is not covered:
- If you only want the GLP-1 to lose weight (no qualifying comorbidity), Medicare does not cover that. The law (Medicare Modernization Act of 2003) explicitly excludes drugs “when used for weight loss, weight gain, or anorexia.” (ASPE)
- Some proposed changes (including reinterpreting the exclusion for obesity) were considered, but in April 2025 those were not finalized. (Medicare Policy Initiative)
FDA approvals matter: When a GLP-1 drug gains an FDA label for something like reducing heart attack risk (beyond weight loss), that opens up possible Medicare Part D coverage for that use. But coverage and cost still depend on your specific Part D plan’s formulary, tiering, prior authorization rules, etc. (KFF)
What Are GLP-1 Drugs Really?
To understand whether it’s a good move, it helps to know what GLP-1s are and how they work:
GLP-1 (Glucagon-Like Peptide-1) receptor agonists are hormones or synthetic mimics that help your body in multiple ways:
- Increase feelings of fullness / reduce hunger.
- Slow gastric emptying (food stays longer in stomach), so you feel satisfied longer.
- Improve how your body handles insulin / blood sugar (very helpful in type 2 diabetes).
Some of the brand names: Wegovy, Ozempic, Zepbound, Mounjaro. Doses, formulations, and FDA-approved uses differ among them. Sometimes the same active chemical is used under different brand names for different conditions (e.g. for diabetes vs. obesity vs. cardiovascular risk).
Pros & Cons: What to Weigh
Here are the upsides and risks—so you (and your doctor) can decide carefully.
| Pros | Cons & Risks |
|---|---|
| Significant weight loss for many people (often more than older weight-loss medications) | Side effects: nausea, vomiting, diarrhea or constipation, possible gallbladder disease, rare but serious risks (e.g. pancreatitis) |
| Improved outcomes for diabetes (better blood sugar), cardiovascular benefits in certain patients (e.g., Wegovy’s FDA approval for reducing heart attack/stroke in people with obesity + CV disease) | Cost is extremely high (often $1,000+ per month without discounts), copays or deductibles vary depending on plan |
| Potential improvements in sleep apnea, joint pain, mobility, quality of life if weight comes down | Many will regain weight when the drug is stopped; requires commitment and sustained lifestyle change |
| Reduced risk for obesity-related illnesses (e.g. certain kinds of liver disease, high blood pressure, joint wear & tear) | Long-term effects still being studied; not enough data yet on outcomes after years or decades for all populations (older adults especially) |
Why Diet + Exercise Still Matter (for Most People)
Medication can be useful, but it’s not magic. Here’s why lifestyle remains foundational:
- Lower risk of side effects vs. medication. Good nutrition + physical activity carry far fewer adverse risks.
- Builds sustainable habits: muscle, mobility, stamina, mental well-being. Even modest weight loss (5-10%) through lifestyle changes can lead to meaningful health benefits.
- Cost effectiveness: healthy eating, activity, small behavior changes are usually much less expensive—and more within people’s control.
- Improves overall health beyond weight: better sleep, mood, cardiovascular health, balance, risk of falls, cognitive health.
What Changes Might Be Coming & What to Watch
This is not static—things are shifting. Keep your eyes peeled for:
- Proposed rule changes: There was a proposal to reinterpret the Medicare exclusion for anti-obesity drugs so that obesity itself (not just when comorbid with another condition) might be considered a “medically accepted indication.” But that change was not finalized in April 2025. (Medicare Policy Initiative)
- Pilot programs: There have been reports that experiments or pilot programs are being considered to allow Medicare and Medicaid to better cover GLP-1s for obesity (possibly starting 2026/2027) in certain states or under certain conditions. But nothing universal yet. (CMS)
- Formularies and plan differences: Even when Medicare can cover, which Part D plan you have makes a big difference. Drugs may be on the formulary, but high cost tiers, prior authorizations, or restrictive access may reduce actual access.
What You Should Do If You’re Considering GLP-1s
Here’s a roadmap to help you decide, in a grounded, safe, informed way:
- Talk to your doctor ABOUT all your health conditions. If you have cardiovascular disease, diabetes, sleep apnea, or other eligible diagnosis, ask whether GLP-1 might be appropriate for that indication.
- Verify your Part D plan’s formulary — find out if your specific drug is covered under your plan, what tier, what your copays/deductibles will be, and what prior authorizations are required.
- Compare costs vs. benefits for your situation. If you’re paying thousands out of pocket, what extra health benefit are you getting—and does that justify the cost (financially & risk-wise)?
- Don’t stop lifestyle work. Even if on a drug, diet, exercise, sleep, stress management still matter hugely. The drug helps but isn’t a replacement for healthy habits.
- Plan for the long haul: Be aware what happens if you stop the medication. Some weight regain often occurs. Also be aware of long-term safety questions and make sure your provider is monitoring you carefully.
- Stay informed: Medicare laws, FDA indications, coverage rules are changing. If a proposed rule becomes final, you may get more coverage. I can help track those changes for you.
Final Word (With Heart)
I get it. This is personal. Weight, health, aging—they’re sensitive. It’s tempting to view a drug like a shortcut, especially when everyone seems to be talking about it. And for some people, these GLP-1s are life-changing.
But for many, especially people without qualifying conditions, it makes sense to be extremely cautious:
- Because Medicare right now will pay only in certain cases (not for weight loss alone).
- Because side effects are real, costs are high, and long-term data is still evolving.
- Because the habits you build through good food, moving your body, resting well—those tend to carry forward long after medicines stop.
Perfect idea — adding FAQ boxes will make your GLP-1 Medicare article skimmable and extra helpful. Here’s a set you can drop right into the post:
GLP-1 & Medicare FAQ
No. Medicare law still excludes drugs prescribed only for weight loss. Coverage is limited to FDA-approved uses like type 2 diabetes, reducing cardiovascular risk, or treating sleep apnea.
- Ozempic® / Mounjaro® – when prescribed for type 2 diabetes.
- Wegovy® – if prescribed for cardiovascular risk reduction in adults with obesity/overweight + established heart disease.
- Zepbound™ – if prescribed for obstructive sleep apnea in adults with obesity.
Coverage still depends on your Part D plan formulary and may require prior authorization.
Retail prices often exceed $1,000 per month. Even with coverage, you may face deductibles, copays, or step therapy depending on your Part D plan.
Common side effects include nausea, diarrhea, constipation, and vomiting. Some people develop gallbladder problems or rarely, pancreatitis. Many regain weight if they stop taking the drug. Long-term safety data in seniors is still limited.
For many, yes. Even a modest 5–10% weight loss through lifestyle change can improve blood pressure, blood sugar, cholesterol, sleep, and mobility — all with far fewer side effects and costs. GLP-1 drugs can help certain patients, but lifestyle remains the foundation for long-term health.
Possibly. Bills like the Treat and Reduce Obesity Act would allow Part D to cover FDA-approved weight-loss drugs more broadly, but as of late 2025, no such law has passed.