You might wonder if Medicare will pay for meals delivered to your home. Original Medicare (Parts A and B) usually does not cover home meal delivery, but some Medicare Advantage (Part C) plans and special programs can include limited meal delivery benefits under certain medical or post-hospital conditions.
This article will walk you through which plans may help, when coverage can apply, and what to ask about eligibility.
You can get clear answers and one-on-one help from The Modern Medicare Agency. Our licensed agents explain your options, compare Medicare Advantage benefits that might include meal delivery, and help find plans that fit your needs and budget without extra fees.
Medicare Coverage Basics for Meal Delivery
Medicare usually does not pay for meals delivered to your home, but some plans and situations may offer limited help. Know how eligibility works, what types of services may be covered, and how programs define “meal delivery” so you can make the right choices.
Eligibility Criteria
Original Medicare (Part A and Part B) generally does not cover home meal delivery. Part A does pay for meals only while you are an inpatient in a hospital or skilled nursing facility.
That means if you leave the facility, those inpatient meals stop. Medicare Advantage (Part C) plans sometimes offer meal delivery as a supplemental benefit.
Coverage varies by plan and by state. Plans often limit meals to short-term needs after a hospital or skilled nursing stay, or to members with certain health risks.
You may also qualify for meal delivery through Medicaid or local programs if you meet income or disability rules. Check your plan documents or call your plan’s member services to confirm specific rules, eligibility windows, and any required documentation.
Covered Services Overview
When meal delivery is covered, plans typically pay for prepared meals or meal kits for a set number of days. Coverage might include a set number of meals per day and a total number of days after hospital discharge.
Some plans partner with community groups to provide meals. Expect rules on medical necessity and discharge status.
Coverage may require proof you cannot prepare meals safely or that you have limited mobility. Cost-sharing varies: some Medicare Advantage plans include the benefit at no extra cost, while others may charge a copay or count the service toward a benefit limit.
Always confirm which foods fit your health needs (diabetic, low-sodium) and whether special diets are available under your plan.
Meal Delivery Definitions
“Meal delivery” can mean different things. Common types include:
- Prepared meals: fully cooked, heat-and-serve dishes delivered to your door.
- Meal kits: pre-portioned ingredients and recipes you assemble and cook at home.
- Community-delivered meals: nonprofit or local programs that bring meals to seniors.
Plans may define service by who delivers it, where it’s prepared, and whether a caregiver must be present. Definitions affect whether a plan covers the cost.
The Modern Medicare Agency helps you compare these definitions across plans. Our licensed agents talk with you one-on-one, find Medicare packages that match your needs, and help avoid unnecessary fees so you get clear, affordable coverage.
Original Medicare and Meal Delivery
Original Medicare generally does not pay for meals delivered to your home. You get hospital meals covered when you are an inpatient, but home-delivered food is not a standard benefit.
If you want meal delivery coverage, you usually must look at Medicare Advantage or other programs.
Medicare Part A and Hospital Meals
Medicare Part A covers meals when you are an inpatient at a hospital or a skilled nursing facility following a qualifying hospital stay. That means while you are officially admitted, the hospital provides meals and Medicare pays for them as part of your inpatient care.
Part A does not cover meals once you leave the facility. It also does not pay for food you buy and bring home after discharge.
If you need short-term meal support after a hospital stay, ask the hospital discharge planner about transitional services; sometimes Medicare pays for medically necessary home health services, but not routine food delivery.
Medicare Part B Coverage Limitations
Medicare Part B focuses on outpatient medical services and does not cover routine meal delivery. It will pay for nutrition counseling by a qualified provider if you have certain conditions, like kidney disease or diabetes, and that counseling addresses medical needs rather than meal costs.
Part B may cover durable medical equipment and some home health services when ordered by a doctor and medically necessary. Those services can include skilled nursing or therapy visits, but they do not include paying for regular grocery or prepared-meal delivery.
For meal help beyond what Original Medicare offers, you can explore Medicare Advantage plans, Medicaid, or local charities.
Medicare Advantage Plans and Meal Delivery Services
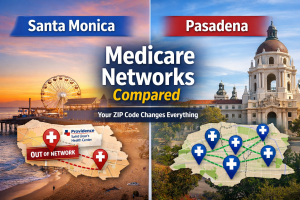
Medicare Advantage plans can sometimes pay for home-delivered meals, short-term or ongoing, and the availability depends on plan and location. You should check which plans in your county offer meal benefits, how many meals they provide, and whether you qualify for them.
Supplemental Benefits for Nutrition
Medicare Advantage plans call extra offerings “supplemental benefits.” These can include daily delivered meals after a hospital stay, or a monthly meal allowance for chronic conditions.
Some plans give 7–14 prepared meals after discharge; others offer a set number per month like 28 meals. Coverage often targets people with specific medical needs, recent inpatient care, or limited ability to cook.
Ask the plan for details: number of meals, meal type (fresh vs. frozen), dietary options, delivery fees, and whether a clinician must certify need. If you have dietary restrictions—diabetic, low-sodium, or pureed—confirm the plan’s vendors can meet them.
How to Find Plans That Cover Meal Delivery
Start by entering your ZIP code on Medicare’s plan finder or calling 1-800-MEDICARE to see local options. Look for plan documents named “Evidence of Coverage” and “Summary of Benefits” and search for keywords like “meals,” “home-delivered meals,” or “nutrition.”
Compare how many meals are included, any cost sharing, and time limits. You can also contact The Modern Medicare Agency.
Our licensed agents speak with you one-on-one, review plans available in your area, and match coverage to your needs without extra fees. They explain meal limits, vendor rules, and enrollment steps so you pick a plan that fits your budget and health needs.
Enrollment Periods and Coverage Changes
You can enroll in a Medicare Advantage plan during Initial Enrollment, Annual Election Period (Oct 15–Dec 7), or a Special Enrollment Period if you qualify. Meal benefits can change each plan year; insurers update supplemental benefits during open enrollment.
A plan that covered meals last year might reduce or remove that benefit for the next year. Before you switch, check the plan’s current year benefit files and ask The Modern Medicare Agency’s agents to confirm meal delivery terms for the new plan year.
If a plan drops meal coverage after you enroll, agents can help you evaluate other plans or options during allowed enrollment periods.
Special Circumstances and Meal Delivery
Some Medicare plans offer temporary or targeted meal help when you leave the hospital or manage a long-term health condition. These benefits vary by plan, time limit, and medical need, so check specifics with your plan or a licensed agent.
Post-Discharge Meal Benefits
After a hospital stay, some Medicare Advantage plans provide meal delivery for a short time to help you recover at home. Typical offers include a set number of prepared meals for 7–14 days or a grocery allowance to cover nutritious foods.
These benefits aim to reduce readmission risk by improving nutrition and easing the transition from hospital to home. To get this benefit, you usually need to be discharged from an inpatient stay and have it listed as a post-discharge service in your plan’s Summary of Benefits.
Contact your plan quickly—some benefits must be requested before or immediately after discharge. The Modern Medicare Agency can check plan details for you and connect you to a licensed agent who explains timing, meal counts, and whether delivery is via a vendor or local program.
Chronic Condition Support Options
If you have a chronic condition, certain Medicare Advantage plans and Special Needs Plans may include ongoing meal support tied to your diagnosis. These benefits typically require documentation that meals are part of your care plan for diabetes, heart failure, or other chronic illnesses.
Coverage can include weekly meal deliveries, nutrition counseling, or grocery credits. Plans differ in length and frequency of meals and may limit which conditions qualify.
You should ask for written plan rules and any medical eligibility criteria. The Modern Medicare Agency’s licensed agents review your health needs and find plans that match your condition without extra fees.
They talk with you one-on-one to explain how chronic-care meal benefits work and how to apply or submit provider documentation.
Types of Meal Delivery Services Available to Seniors
You can get meals that match medical needs or choose between ready-to-eat dishes and do-it-yourself kits. Each option affects cost, nutrition, and how much you need to cook or heat.
Medically Tailored Meal Programs
Medically tailored meals are made to match a diagnosed condition, such as diabetes, heart disease, or kidney disease. Meals follow specific calorie, sodium, and nutrient limits set by dietitians or doctors.
You may receive several meals per week, often delivered chilled or frozen so you just heat and eat. Coverage varies: Original Medicare usually won’t pay for these, but some Medicare Advantage plans or local programs may help if a doctor documents medical need.
Check plan benefits carefully and keep prescriptions or dietitian notes ready. The Modern Medicare Agency can help you review plans and confirm whether a Medicare Advantage option covers medically tailored meals for your condition.
Meal Kits Versus Prepared Meals
Meal kits provide pre-measured ingredients and recipes so you cook at home. They give control over fresh ingredients and portion size but require time and basic cooking skills.
Kits can suit people who want involvement in meal prep and can follow simple recipes. Prepared meals arrive fully cooked and only need reheating.
They save time and reduce fall or injury risk for people with limited mobility. Prepared meals often include clear nutrition labels and portion-controlled servings.
Some Medicare Advantage plans may cover short-term prepared meals after a hospital stay. Talk with The Modern Medicare Agency to find plans that match whether you prefer kits or ready-made meals and to learn about plan rules, copays, and any eligibility you must meet.
Other Resources for Senior Meal Assistance
You can find help through state programs that may pay for meals and through local groups that deliver food. Check eligibility rules, local availability, and how long benefits last before you sign up.
Medicaid and Dual Eligibility
If you have Medicaid or both Medicare and Medicaid (dual eligible), you may qualify for meal benefits that Medicare alone won’t cover. Medicaid rules differ by state, but many state Medicaid programs include home-delivered meals or a short-term meal benefit after a hospital or nursing stay.
Contact your state Medicaid office to ask about covered services, eligibility criteria, and how to apply. If you are dual eligible, your state Medicaid plan may fill gaps in Medicare coverage, such as home meal delivery, grocery allowances, or nutrition counseling.
Keep records of doctor notes or discharge paperwork, because some programs require medical need documentation.
Community and Nonprofit Programs
Local nonprofits and community groups often run meal delivery programs for seniors. Meals on Wheels and senior centers commonly provide hot meals, frozen meals, or grocery delivery based on need and mobility.
Find programs by calling your local Area Agency on Aging or 211. Ask about eligibility, donation suggestions, delivery schedules, and whether volunteers will provide social checks during delivery.
If you need help navigating options or applying, The Modern Medicare Agency can connect you with a licensed agent. Our agents speak with you one-on-one, match Medicare plans to your needs, and won’t add hidden fees.
Tips for Navigating Meal Delivery Coverage
You should know how to challenge denials and how to get doctors and case managers to support meal delivery requests. These steps increase the chance you get covered meals when you meet plan rules or need short-term help after a hospital stay.
Appealing Coverage Denials
If a plan denies meal delivery, start by reading the denial letter carefully. Note the exact reason, the deadline to appeal, and any documents the plan asks for.
Gather proof such as doctor notes, hospital discharge papers, and records showing limited ability to prepare food. Ask your doctor to write a short statement that links the meal need to a medical condition or recovery plan.
Submit the statement with your appeal form. Keep copies of everything.
Follow the plan’s appeal timeline exactly. Call customer service to confirm receipt and ask for a case number.
If the internal appeal fails, you can request an external review from your state or a federal reviewer. Keep a log of calls, names, and dates.
Coordinating With Healthcare Providers
Talk with your primary care doctor, case manager, or discharge planner before leaving the hospital. Ask them to document specific medical reasons why meal delivery helps your recovery or prevents readmission.
Request concise, written orders or notes that state how many meals per day and for how long you need them. That detail helps a Medicare Advantage plan or a reviewer see the medical necessity.
Share these notes with your plan and with The Modern Medicare Agency agent you speak with. Use your agent at The Modern Medicare Agency to match your documented needs to plans that commonly offer meal benefits.
Our licensed agents talk with you one-on-one and help submit paperwork without extra fees. This saves time and reduces mistakes that can cause denials.